Diseases & Conditions
Distal Radius Fractures (Broken Wrist)
A fracture of the distal radius occurs when the radius — one of the two long bones in the forearm — breaks close to the wrist.
Distal radius fractures are very common. In fact, the radius is the most commonly broken bone in the arm.
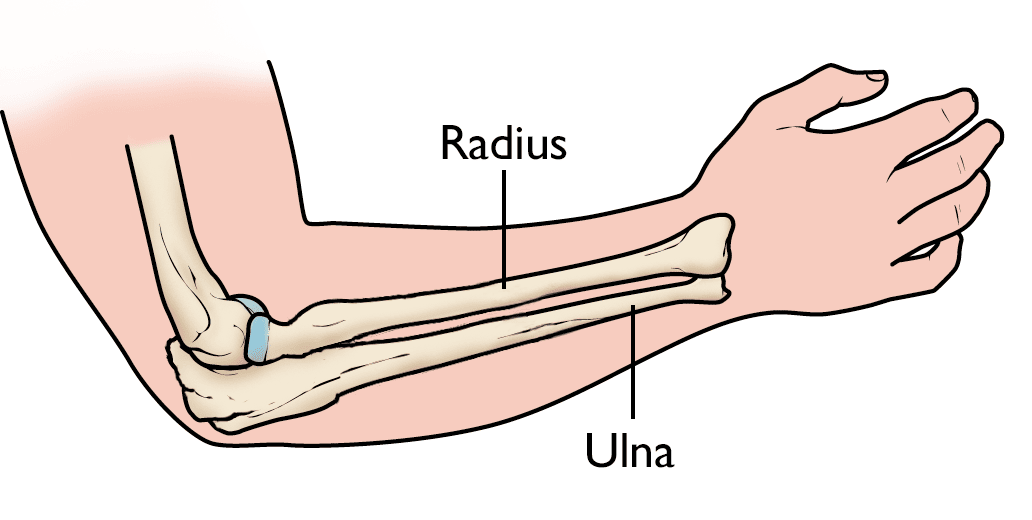
Anatomy
There are two long bones that make up the forearm:
- The radius is on the thumb side of the forearm.
- The ulna is on the small finger (pinky) side.
At the proximal forearm, the part of the forearm closest to the elbow, the ulna is larger. At the distal forearm, the part of the forearm closest to the wrist, the radius is larger.
Description
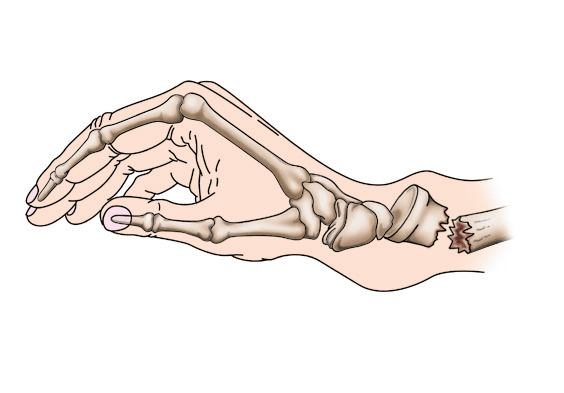
A distal radius fracture almost always occurs about 1 inch from the end of the bone. This very common fracture can occur in many different ways to people of all ages. In young people, such fractures typically occur in high-energy accidents, such as a fall from a ladder or a car crash. In older people, especially those with osteoporosis, distal radius fractures can occur from a simple fall onto the wrist.
One of the most common distal radius fractures is a Colles fracture, in which the broken fragment of the radius tilts upward. This fracture was first described in 1814 by an Irish surgeon and anatomist, Abraham Colles — hence the name Colles fracture.
Other ways the distal radius can break include:
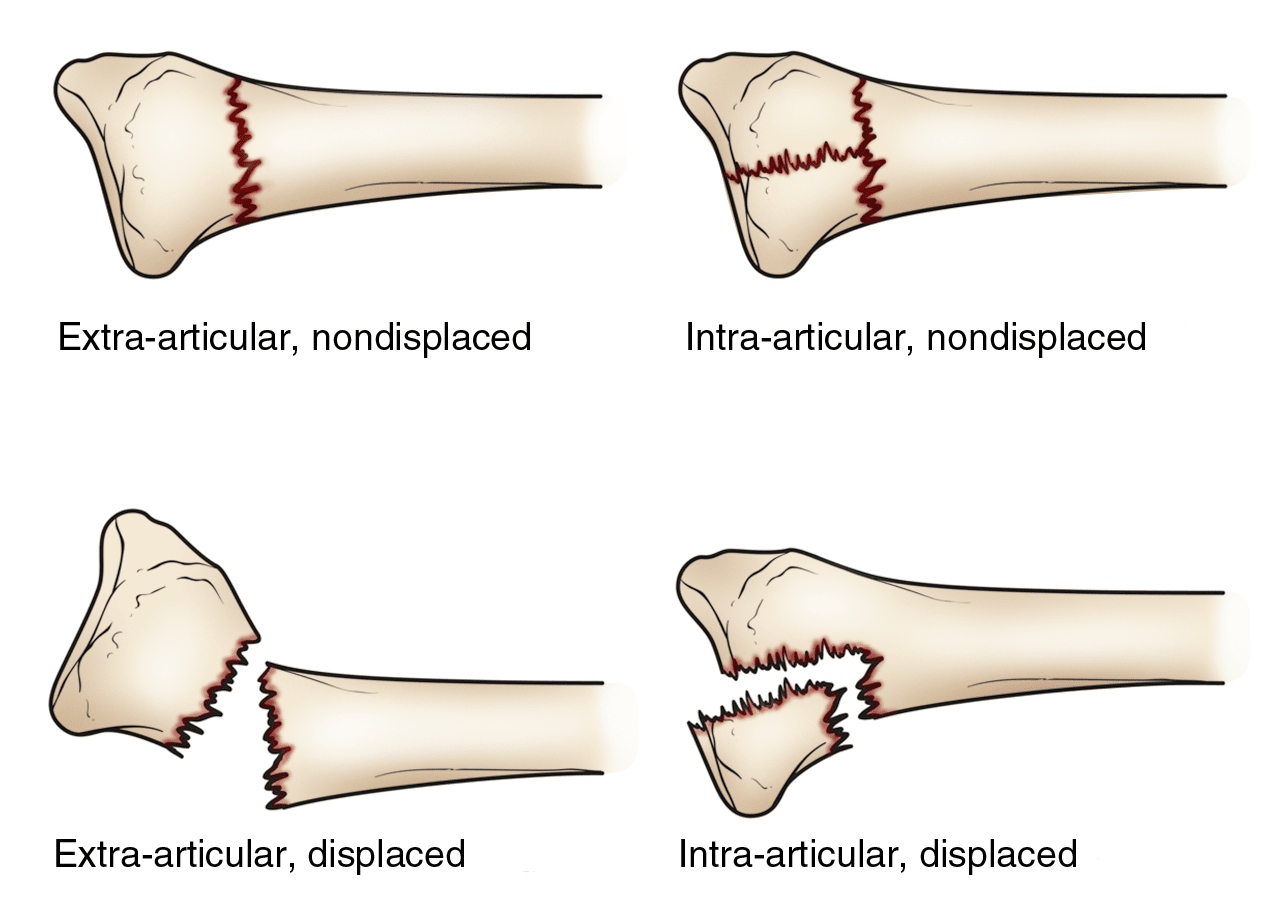
- Intra-articular fracture — An intra-articular fracture is one that extends into the wrist joint. ("Articular" means "joint.")
- Extra-articular fracture — A fracture that does not extend into the joint is called an extra-articular fracture.
- Open fracture — When a fractured bone breaks the skin, it is called an open fracture. These types of fractures require immediate medical attention because of the risk of infection.
- Comminuted fracture — When a bone is broken into more than two pieces, it is called a comminuted fracture.
It is important to classify the type of fracture because intra-articular fractures, open fractures, comminuted fractures, and displaced fractures (when the broken pieces of bone do not line up straight) are more difficult to treat than other types of fractures.
Sometimes, the other bone of the forearm (the ulna) is also broken. This is called a distal ulna fracture. Depending on the type of distal ulna fracture, you may or may not require additional treatment.
Cause
The most common cause of a distal radius fracture is a fall onto an outstretched arm.
Osteoporosis (a disorder, common in older adults, in which bones become very fragile and more likely to break) can make a relatively minor fall result in a broken wrist. Many distal radius fractures in people over the age of 60 are caused by a fall from a standing position.
A broken wrist can happen even in healthy bones if the force of the trauma is severe enough. For example, a car accident or a fall off a bike may generate enough force to break a wrist in a young and healthy person.
Symptoms
A broken wrist usually causes immediate pain, tenderness, bruising, and swelling. In many cases, the wrist hangs in an odd or bent way (deformity).
In very severe fractures, the nerve(s) to the hand can be affected by the injury, resulting in numbness in the fingers. If you experience numbness in your fingers after a wrist injury, go to an urgent care center or emergency room right away. The injury may need to be addressed quickly to prevent permanent nerve damage.
Doctor Examination
If the injury is not very painful and the wrist is not deformed, it may be possible to wait until the next day to see a doctor. The wrist may be protected with a splint. An ice pack can be applied to the wrist and the wrist can be elevated until a doctor is able to examine it.
If the injury is very painful, the wrist is severely deformed, or the fingers are numb or pale, go immediately to an urgent care center or emergency room for further treatment.
To confirm the diagnosis, the doctor will likely order X-rays of the wrist. X-rays can show if the bone is broken and whether there is displacement (a gap between broken bones). They can also show how many pieces of broken bone there are.
In some cases, the doctor may order a computed tomography (CT) scan, which provides 3-D pictures of the broken bone. This can help with surgical planning.
Treatment
The treatment of broken bones follows one basic rule: The broken pieces must be put back into position and prevented from moving out of place until they are healed.
There are many treatment options for a distal radius fracture. The choice depends on many factors, such as the nature of the fracture, your age and activity level, and the surgeon's best judgment.
Nonsurgical Treatment
If the broken bone is in a good position, a cast may be applied until the bone heals.
If your broken bone is out of place and likely to limit the future use of your arm, it may be necessary to re-align the broken bone fragments. Reduction is the technical term for the process in which the doctor moves the broken pieces into place. When a bone is straightened without having to open the skin (incision), it is called a closed reduction.
After the bone is properly aligned, a splint or cast may be placed on your arm to keep the bones aligned. A splint is usually used for the first few days to allow for a small amount of normal swelling. A cast is usually added a few days to a week or so later, after the swelling goes down. The cast is often changed 2 or 3 weeks later because as the swelling goes down more, the cast loosens.
Depending on the nature of the fracture, your doctor may closely monitor the healing by taking regular X-rays. In patients treated without surgery, X-rays are often taken at weekly intervals for 3 weeks and then once again at 6 weeks. X-rays may be taken less often if the fracture did not need to be reduced and/or was thought to be stable. If at any time the fracture becomes poorly aligned, surgery may be recommended.
In non-operative fractures, the cast is typically removed about 6 weeks after the fracture happened. At that point, you will likely start physical therapy to help improve the motion and function of the injured wrist. Typically, you will wear a removeable splint between therapy sessions to protect the healing bone.
Surgical Treatment
Sometimes, the position of the bone cannot be corrected with a closed reduction alone and/or cannot or kept corrected in a cast. These fractures may heal in bad alignment, which can result in poor function of your arm. In such cases, you may require surgery to correct the fracture and hold it in place while it heals.
Procedure. Surgery typically involves making an incision on the wrist over the fracture to access the broken bone(s). Important structures such as arteries, nerves, and tendons are identified and protected. The surgeon realigns the broken bone(s) directly through the incision. This process is also known as an open reduction.
Depending on the fracture, there are several options for holding the bone in the correct position while it heals after it has been re-aligned:
- Cast — Casts are rarely used after an open reduction.
- Metal pins (usually stainless steel or titanium) — This treatment was common years ago and is still used frequently in children with growing bones.
- Plate and screws — This is the most common option for surgical treatment of distal radius fractures.
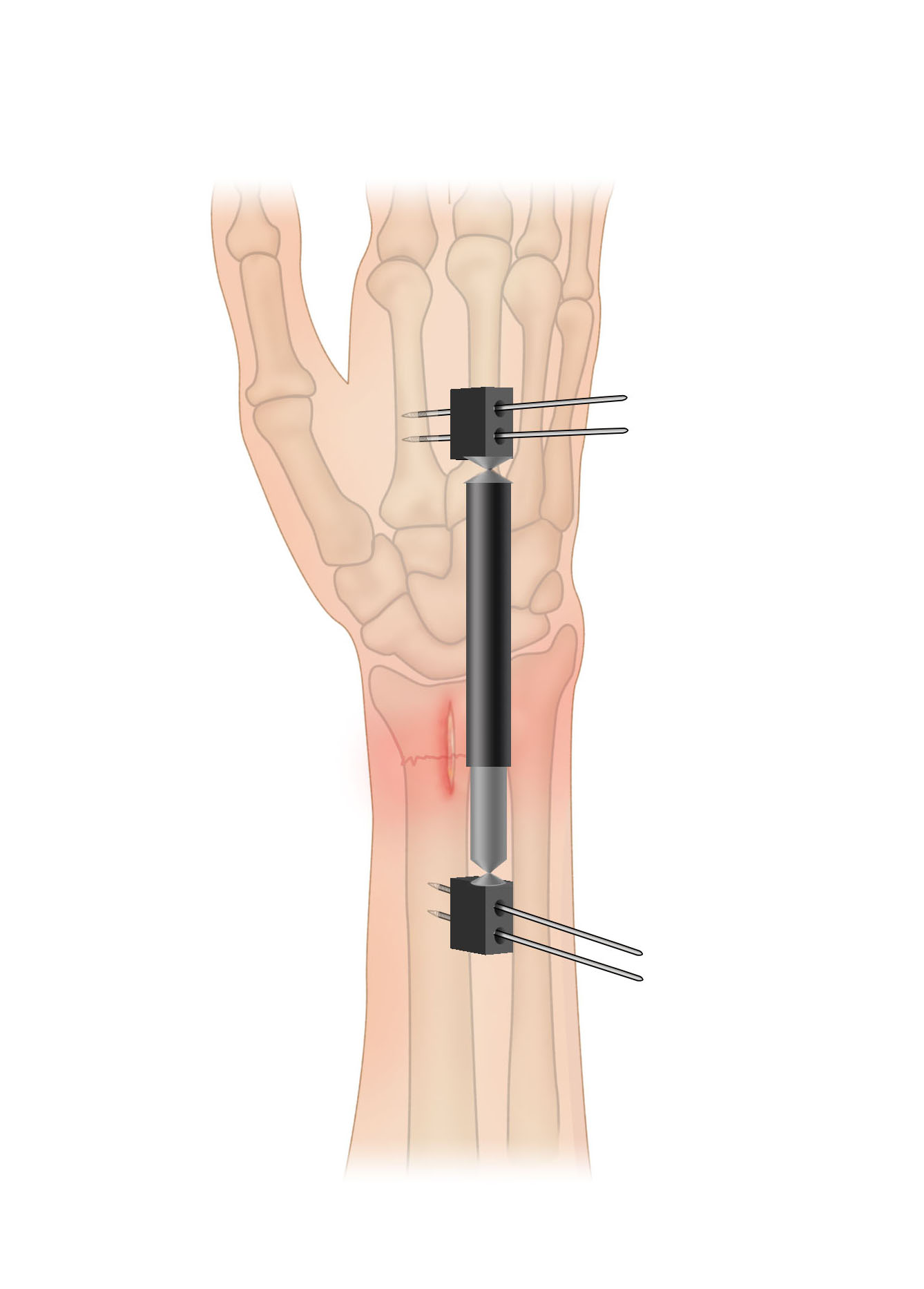
- External fixator (a stabilizing frame outside the body that holds the bones in the proper position so they can heal) — This has become less common in recent years but is still a good option for severe and open fractures.
- Any combination of these techniques
Open fractures. Surgery is required as soon as possible (typically within 24 hours or less after injury) for most open fractures.
- The exposed soft tissue and bone is thoroughly cleaned (debrided) and antibiotics are given to prevent infection.
- Either external or internal fixation methods are often used to hold the bones in place.
- If the soft tissues around the fracture are badly damaged, your doctor may apply a temporary external fixator.
- Internal fixation with plates or screws may be utilized at a second procedure several days later when swelling goes down and the soft tissues around the fracture are ready.
Recovery
Because the kinds of distal radius fractures are so varied and the treatment options are so broad, recovery is different for everyone. Talk to your doctor for specific information about your recovery program and return to daily activities. Most distal radius fractures take 3 months or so to heal before you are able to return to all activities, and full recovery from these injuries can take up to 1 year.
Pain Management
Most fractures hurt moderately for a few days to a couple of weeks. Many patients find that using ice, elevation (holding their arm up above their heart), and non-prescription pain relief medications will effectively relieve their pain.
Your doctor may recommend combining ibuprofen and acetaminophen to relieve pain and inflammation. The combination of both medications is much more effective than either one alone. If pain is severe, your doctor may suggest a prescription-strength medication, such as an opioid, for a few days.
Be aware that although opioids help relieve pain after surgery, they are narcotics and can be addictive. It is important to use opioids only as directed by your doctor and to stop taking them as soon as your pain begins to improve. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Cast and Wound Care
In some cases, original casts will be replaced because swelling has gone down so much that the cast becomes loose. For non-operative fractures, the last cast is usually removed after about 6 weeks.
During healing, casts and splints must be kept dry. A plastic bag over the arm while showering should help. If the cast does become wet, it will not dry very easily. A hair dryer on the cool setting may be helpful. Often, the cast needs to be replaced if it becomes wet.
Most surgical incisions must be kept clean and dry for at least 5 days. Your doctor will tell you when it is OK to remove the bandages after your surgery.
Potential Complications
After surgery or casting, it is important that you achieve full motion of your fingers as soon as possible. If you are not able to fully move your fingers within 24 hours due to pain and/or swelling, contact your doctor for evaluation.
Your doctor may loosen your cast or surgical dressing. In some cases, you will need to work with a physical or occupational therapist to regain full motion.
Unrelenting (constant) pain may be a sign of complex regional pain syndrome (reflex sympathetic dystrophy), which must be treated aggressively with medication or nerve blocks. Notify your doctor if you have extreme pain that does not become less severe with medication.
Rehabilitation and Return to Activity
Most people do return to all their former activities after a distal radius fracture. The nature of the injury, the kind of treatment received, and the body's response to the treatment all have an impact. In some cases, you can experience permanent limitations in function after such injuries.
Almost all patients will have some stiffness in their wrist. This will generally lessen in the month or two after the cast is taken off or after surgery and continue to improve for at least 2 years. If your doctor thinks it is needed, you will start physical therapy within a few days to weeks after surgery, or right after the last cast is taken off.
Most patients will be able to resume light activities, such as swimming or exercising the lower body in the gym, within 1 to 2 months after the cast is removed or within 1 to 2 months after surgery. Vigorous activities, such as skiing or football, may be resumed between 3 and 6 months after the injury.
Long-Term Outcomes
Recovery should be expected to take at least 1 year.
Some pain with vigorous activities may be expected for the first year. Some residual stiffness or ache is to be expected for 2 years or possibly permanently, especially for high-energy injuries (such as motorcycle crashes), in patients over the age of 50 years, or in patients who have osteoarthritis. However, the stiffness is usually minor and typically does not affect the overall function of the arm.
Finally, osteoporosis is a factor in many wrist fractures. It has been suggested that most people who have a wrist fracture should be tested for bone weakness, especially if they have other risk factors for osteoporosis (e.g., older age). Ask your doctor about osteoporosis testing.
For more information, watch: Distal Radius Fractures (Broken Wrist) Overview
To assist doctors in the management of distal radius fractures, the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Plain Language Summary- Clinical Practice Guideline - Distal Radius Fractures - AAOS
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.